What Is an EMR and EHR?
An EMR is an electronic medical record and an EHR is an electronic health record. Both can be a part of medical records management. An EMR is usually a record within a single provider’s office. An EHR,however, is more comprehensive, and patients can use it across health organizations. Typically EHRs can move with a patient, while EMRs cannot.
What Is Medical Records Management?
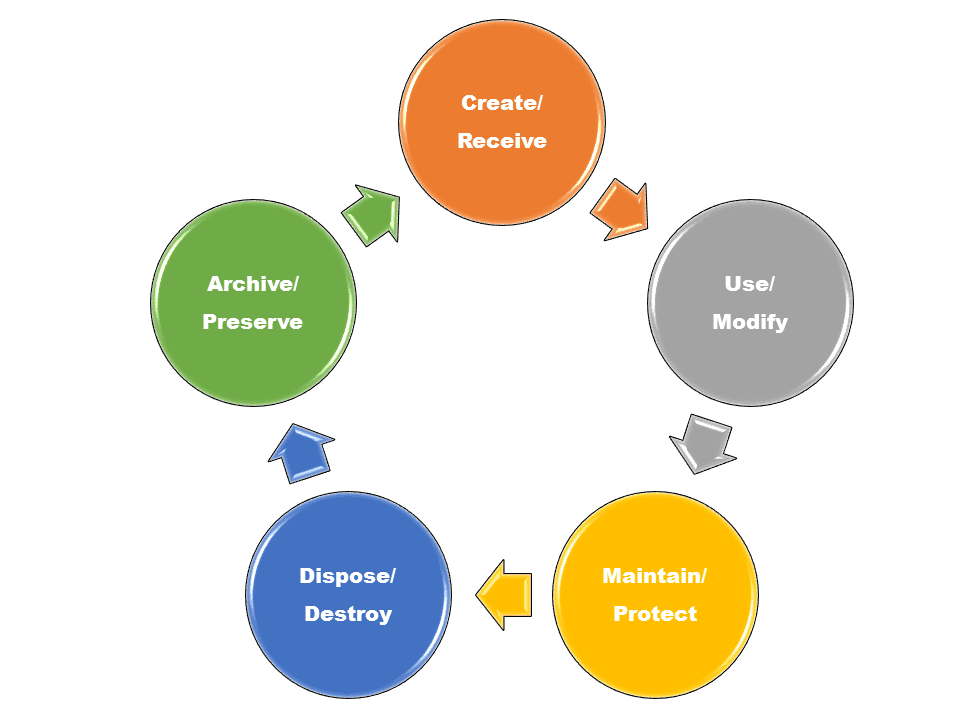
Medical records management is the part of records management that relates to the operation of a healthcare practice. It is the field of management that is responsible for all records throughout their lifecycle from creation, receipt, maintenance, and use to disposal. For an in-depth look at records management, read Records Management: Maintaining Your Organization's Information.
Sometimes referred to as health information management (HIM) or health records information management (HRIM), medical records management can involve anything and everything about a practice and a patient, including but not limited to a patient’s history, clinical findings, diagnostic test results, pre- and postoperative care, patient progress, and medications.
A medical record can help both the physician and the patient. For the patient, the record can outline one’s history and treatment plan in an easily-accessible way. For the physician, it can provide support about the correctness of that treatment plan. A good medical records management system can be the difference between life and death if someone needs to check a test, a medication, or make a quick medical decision.
Benefits of Medical Records Management
As the requirements for medical records change, it is important for medical practices, hospitals, skilled nursing facilities, and long-term care facilities to have a medical records management system in place that includes automating, capturing, storing, and disseminating records. The system improves record location and tracking, even for records people don’t frequently use. It can also preserve historical and vital information about a medical facility in case of a disaster or legal requirement.
A records management system can also make it easy to transfer or release information between offices — both patients and physicians can access the information in a timely manner without duplicating efforts. Arguably, this type of visibility can increase patient safety, reduce mistakes, and increase confidence in a treatment plan. From a productivity standpoint, medical records management might address litigation risks, lower operating costs (due to reduced physical storage needs), and boost employee productivity, mobility, and efficiency.
Some medical records management systems will link to patient management systems, allowing connections between billing and other systems. For more about patient management, read How Patient Management Software Improves the Health Care Experience.
Risks of Unmanaged Medical Records
Not having easy access to potentially life-saving or life-changing health information is a significant risk that unmanaged medical records present. A lack of organization with regard to record keeping can also pose a legal threat. Additionally, when staff are constantly struggling to find things, patients might view the lack of structure and policy as a signal that a practice is behind the times.
Inefficiency can also lead to a loss of productivity, duplication of efforts, or an inability to complete necessary tasks. Billing errors could arise as a result of poor records that ultimately cost the practice money. Paper records also require a physical storage area and can sometimes result in practices needing to purchase additional office space, which can be expensive.
When individuals create their own non-standardized systems, they are exposing an organization to more potential issues. For example, it could lead to insufficient backup plans and increased costs to convert records from formats that adhered to technology that eventually became obsolete. Simply having backups of data in multiple places is pointless if it is not accessible or usable.
Unfortunately, many medical facilities do not see medical records management as a critical or necessary function. As a result, they do not provide training or structure to create an efficient and compliant policy.
What Is the Difference Between Electronic Medical Records (EMR) and Electronic Health Records (EHR)?
Both the EMR and EHR contain electronic versions of a patient's medical history. Most of the information in an EMR goes into an EHR.
|
EMR vs. EHR: Similarities and Differences |
|
|
EMR (electronic medical record) |
EHR (electronic health record) |
|
Medical and clinical data gathered in one provider’s office |
Medical and clinical data gathered from many providers’ offices and hospitals |
|
Narrower view |
Broader view |
|
Digital version of a paper chart in one office |
Digital version of varied health information |
|
Not designed for sharing |
Designed for sharing outside of an individual medical practice |
|
Providers use mainly for diagnosis and treatment |
Providers have access to many diagnostic tools to make decisions |
The EMR can contain medical history, diagnoses, medications, immunizations and dates, allergies, etc. Often, a patient needs to ask for a printed copy of an EMR to share with another medical provider.
The EHR contains similar details as the EMR, but also other relevant data like information from wearable devices, demographics, and insurance information. It can also contain lab data and imaging reports that come from other offices or practices. Assuming the software is compatible, other offices and practices can access the information within an EHR to help coordinate care and make clinical decisions.
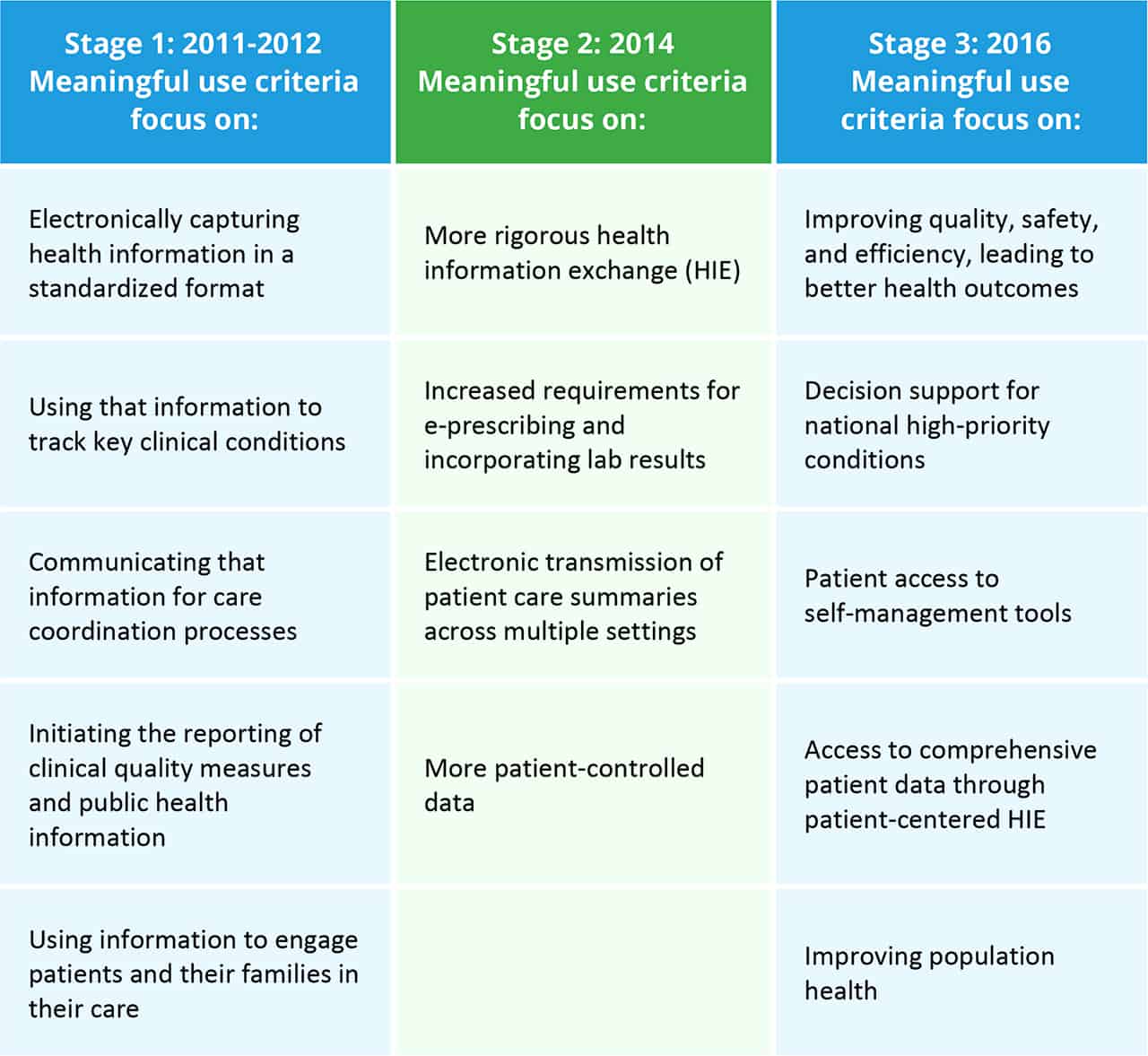
To receive reimbursements from Medicare and Medicaid, medical practices may need to follow a set of criteria called Meaningful Use requirements. This criteria involves using EHR technology to engage patients and families, improve safety, efficiency, and quality, reduce health disparities, improve care coordination and overall population and public health, and maintain privacy and security of patient health information. Incentive programs came with the initial phase-in of the criteria in 2011 and improved outcomes were supposed to occur during the following five years.
Source: Office of the National Coordinator for Health Information Technology - U.S. Department of Health and Human Services
The term EHR is becoming more widely-used because it is more comprehensive. Additionally, practices may need to adopt the EHR in order to qualify for Medicare and Medicaid reimbursement.
“An electronic health record is constantly evolving,” Kadlec says. “In the past, it was just a repository of information. Now it is a living and evolving story of a patient’s health.” The field of health information management has evolved along with it. The data that is now part of a record has grown from just symptoms, diagnoses, and treatments to include billing data, records of visits, images, and more.
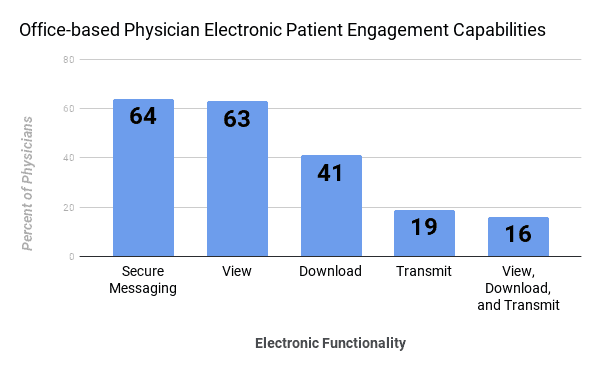
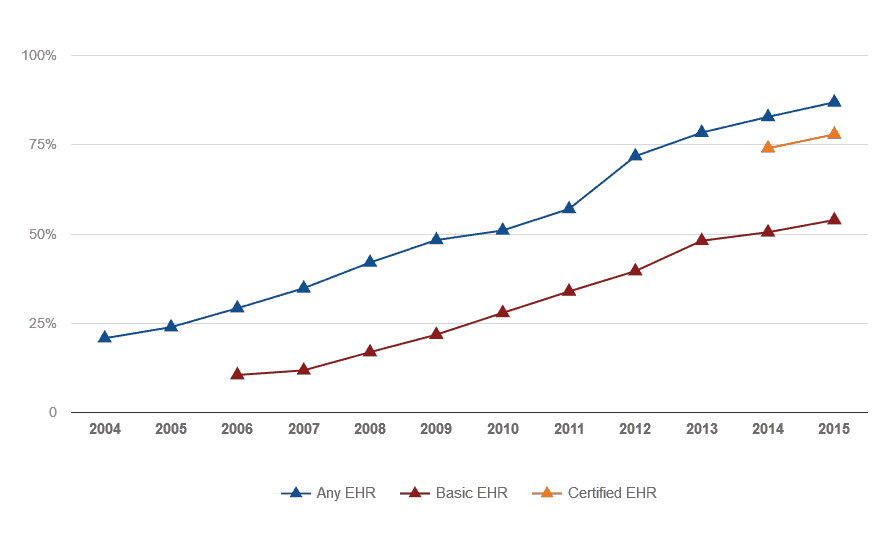
Data from a 2015 survey showed that usage of EHRs is increasing, allowing patients to meaningfully engage with their healthcare providers. However, there is still a long way to go until all practices are using fully-functional EHR systems.
In the 2015 survey, 64 percent of physicians had an EHR system capable of exchanging secure messages with patients, 63 percent allowed patients to view their EHR, 41 percent allowed patients to download their EHR, 19 percent of systems allowed patients to send their medical record to a third party, and only 16 percent of systems allowed all three functions. The EMR and EHR need to be part of a medical facility’s records management plan.
Source: Office of the National Coordinator for Health Information Technology. 'Office-based Physician Electronic Health Record Adoption,' Health IT Quick-Stat #50 - December 2016
Douglass now uses the term “intelligent health records” to refer to the way some practices currently use EHRs. Features in his company’s and other systems called clinical decision supports can help physicians with diagnoses. Douglass uses an example of a doctor seeing a diabetic patient in the office: The system alerts the doctor that the patient has not had a foot exam or a vision test in 18 months, both of which are important to the overall health of a diabetic. After receiving the alert, the doctor can either do the tests or schedule them while the patient is still in the office. “It’s a way of getting out in front of these problems,” says Douglass.
What Is a Personal Health Record (PHR)?
A PHR is a personal health record, which individuals can use to track their own health information. Some people find them especially useful during treatment for a long-term illness or complicated medical problem.
Typically a PHR includes copies of paper records in a three-ring binder or accordion file. But now there are also applications to help track personal health information electronically. The apps can often accept information from wearable devices and scanned documents. Your PHR will contain sensitive information, so consider the security of whichever system you choose because protecting that data could be crucial.
“There are things that go into your health that aren’t part of your health care,” Kadlec says. “Personal health records are so important - it’s ownership over your own health care.”
For example, if you get a flu shot, it might not become part of your EHR, since many places offer flu shots, not just doctors’ offices. So, including the date and type of shot as part of your PHR is important, as it becomes a reminder to tell your doctor about it at your next appointment, Kadlec explains.
Most PHRs do not connect to employers, health systems, or insurers, but some can connect to physicians’ offices through patient portals. Regardless of how you choose to keep your personal health information, you may consider keeping records of the following:
- Current medications and pharmacy information
- Immunizations
- Allergies
- Health history (including past procedures, surgeries, illnesses, and family history)
- Test and lab results
- Insurance paperwork
- Bills and receipts
AHIMA has a website dedicated to personal health records. Kadlec recommends finding a system that works for you and keeping it updated. “You are the most important person in your own health care. Be your own advocate and be in charge of your own health information,” she says.
Under United States federal law, patients have certain rights regarding access to their medical records from doctors’ offices, hospitals, pharmacies, care facilities, and insurers.
What Are the Benefits of Electronic Health Records?
Handling medical records electronically has many benefits over the older paper counterparts. Providers can more easily track data over time and this tracking is often automated. The ability to track this information is important in many situations, including if a doctor wants to identify how a patient is responding to a particular type of treatment. Electronic records can also help identify patients who might be due for preventive visits and screenings.
They also take up less physical space, and since real estate is expensive, this can save a practice money, or provide them with an area that can serve another valuable purpose other than storage.
Even with all the benefits of electronic records, there can be a learning curve. “If a practice has been on paper it’s entire existence, their relationship with electronic health records is very different,” Douglass says. Established physicians who have only used paper and are not comfortable with technology might have a more difficult time adopting electronic records than a new doctor who has grown up with technology.
Additionally, if an established physician wants to sell a practice, there must be electronic records — not paper — Douglass says, adding that paper practices just don’t sell. Electronic records also allow physicians to enter orders for tests automatically and write prescriptions without prescription pads.
What Is Involved In Medical Records Management?
Medical records management involves many kinds of records, including patient charts, x-rays, images, scans, and even emails. Additionally, it involves making sure all of these items are accessible, safe, and secure.
Unless a practice is brand new, there are probably still some paper charts in the office. Deciding what to do with those charts is vital to the success of any medical records management system. Simply scanning them into an electronic format will not necessarily make them easily accessible for people who need them. A company that specializes in this kind of records transfer (from old to new technology) can make sure they are created properly and adhere to best practices, regulations, and retention schedules.
“The transition depends on the organization,” Kadlec says. “Some organizations choose to have a cutoff date and some organizations choose to live in a hybrid world.”
According to AHIMA, the transfer of paper-based charts into electronic ones takes careful coordination. AHIMA states that practices and clinics must consider the following questions:
- Which historical patient information should be available for patient visits during and after the transition?
- What are the best methods of converting this information to the EHR?
- What is the best way to ensure that the converted data and information is of sufficient quality?
- How long should the paper record be available after the conversion?
- How long do paper records need to be kept after the transition to the EHR?
- What is the role of printing and should it be allowed during the transition?
These answers may be different for different types of practices. For example, those specializing in cardiology might need to keep previous test and diagnosis information more readily available than other practices, since they refer to them often to look for anomalies or trends. Results of a one-time test or procedure might not need as much access. Organizations may need to also decide if someone will manually input important data like allergies, procedure history, current medications, etc., into the new or updated system.
“There is definitely not a one-size-fits-all solution,” Kadlec says. “It’s going to vary by system.” Some factors that you may consider, include budget, patient population, and the number of facilities that need access to the information and how often.
Since some medical records link to practice management systems, the revenue cycle and billing could all be part of the same system, making things easier for both patient and practice.
Regulations for Medical Records Management
Regulations for medical records management may evolve over time. A records policy may include standards for implementation and management, and be flexible enough to meet compliance and legal standards.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) as amended by the Health Information Technology for Economic and Clinical Health Act of 2009 (together, the “Act”), promotes the adoption and meaningful use of health information technology, including electronic health records. The Act included a $25.9 billion budget with a larger portion of it going towards increasing the use of EHRs in physicians’ offices and hospitals.
The Act deals with privacy and security concerns related to medical records management. It provides guidance about how to protect health information, and also lists certain penalties for non-compliance (including fines). Under certain circumstances, medical entities may need to report any data breach impacting 500 or more people to the United States Department of Health and Human Services, to the news media, and to the people affected by the data breaches. The Act also addresses how certain practices can share, store, and disseminate health records.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) changed the way the United States evaluates and pays for health care. One of the the requirements is a meaningful use of EHRs. Under MACRA’s Merit Based Incentive Payments System (MIPS), practices may be required to use a certified EHR system. Not all EHR providers are certified. Douglass shares that it took 80 engineers nine months to get Practice Fusion’s system certified.
Other state and federal laws and regulations may also implicate medical records management programs and may need to be considered during the development and implementation process.
How to Begin or Expand a Medical Records Management Program
If you are accepting Medicare or Medicaid, you are probably well into your medical records management program. However, the Medicare EHR Incentive Program ended after the 2016 reporting period.
If you’re looking to expand your program, it may be best to involve different types of people within a medical practice or office. Simply involving technology and records personnel is not enough. Involve physicians, nurses, other medical staff, front office staff, billing, and pertinent personnel in the decision-making processes. Having input about capital expenses and work processes up front can increase buy in from the staff.
Several companies exist to help set up or expand medical records management. Some will scan and convert existing paper charts, while others build the storage and access of paper charts into a new system.
When shopping for software or a medical records management company, there are several things to consider. Here are a few questions you might ask during the process:
- Can different software platforms connect? If the goal is to have patient management software connect to billing software and to EHRs, make sure they communicate.
- Is the platform secure?
- Does the software enable you to be compliant with HIPAA, HITECH, and other regulations?
- Does your staff have the time and training to make the transition?
The big hurdle now is interoperability, Douglass explains. Banks use a standard called Automatic Clearing House (ACH) to conduct transactions between financial institutions. No such standard exists in the business of medical records management, so systems from different companies may not talk with each other. “It will be the mid-2020s before we get to a point where a patient can go to a new doctor and all of their health information will be in a digital format,” Douglass says.
Companies are working on electronic standards for the Consolidated Clinical Document Architecture (CCDA), which are the standards for clinical care summaries, and other important information. Some platforms will create a file or document that you can export from one system into another, but not all platforms read and interpret those files, Douglass explains.
If you decide to scan your own paper charts, you may need to consider whether you’ve captured all of the data necessary to ensure accessibility. That data may include metadata, the unique identification of each record, who created it, and when.
“It has almost no value being scanned into a PDF and left there,” Douglass advises, adding the task of converting records doesn’t need to be daunting. “Don’t think about having to convert that chart that is 150 pages long. Only a few pages are relevant.” You may use the paper chart along with an electronic one during a patient visit and input the necessary data as you go. “Only the bite-sized information is relevant at that moment,” Douglass adds.
Careers and Training in Medical Records Management
Many medical providers make the mistake of assuming that anyone can handle medical records management. This is not the case: It is a specialized and technical field. In some organizations, there are health information technicians who are responsible for compiling and organizing medical records while maintaining confidentiality and security. There are also health information managers who deal more with the overall health information management structure than the day-to-day data entry. Each organization has different titles and job descriptions with varied salary and certification requirements. As with any skilled type of work, training, certifications, and professional organizations are available.
“Our health information professionals have had to evolve, they have to have knowledge” Kadlec says. AHIMA offers several national certifications and trainings as well as journals and blogs. “Your certification really demonstrates your depth of knowledge. As you get to some of the more technical areas of health information management, being able to demonstrate a proficiency is important.”
Having a certification may not always be mandatory, but it can help justify a position to a hiring manager. “You have proven through testing that you have the skills to fulfill that kind of role,” Kadlec explains.
Several schools also offer programs in information management with specialty tracks in medical records.
Medical Records Management with Smartsheet
Empower your people to go above and beyond with a flexible platform designed to match the needs of your team — and adapt as those needs change.
The Smartsheet platform makes it easy to plan, capture, manage, and report on work from anywhere, helping your team be more effective and get more done. Report on key metrics and get real-time visibility into work as it happens with roll-up reports, dashboards, and automated workflows built to keep your team connected and informed.
When teams have clarity into the work getting done, there’s no telling how much more they can accomplish in the same amount of time. Try Smartsheet for free, today.